Questions Related to the Knee
What is Knee arthritis, symptoms and treatment?
Arthritis is a general term meaning joint inflammation. It is a specific type of wear and tear on the joints that affects nearly 21 million Americans. As we age, the chance of developing osteoarthritis increases and is the most common type of arthritis.
Osteoarthritis breaks down the cartilage in joints and can occur in almost any joint in the body. It is most common in the hips, knees, and spine. Cartilage is the rubbery material on the end of the bones that acts as a shock absorber and provides a smooth, gliding surface.
Over time, the cartilage may break down and wear away. This can lead to the bones rubbing together which causes pain, restricts motion of the joint and can be very uncomfortable during many daily activities.
What does arthritis look like?
Normal Knee

There is good space between the bones representing thick, healthy cartilage. There are smooth bone edges.
Knee with Bone-on-Bone Arthritis

This knee is bone-on-bone since the cartilage has completely worn away. As a reaction to the bone not having smooth cartilage covering it, bone spurs have grown on the outside edges.
What are the Symptoms of Osteoarthritis?
- Joints that are sore and achy, especially after activity
- Pain after overuse or when joints are inactive for long periods of time
- Joint swelling
- Joint stiffness
What are the Causes of Osteoarthritis?
There are several factors that lead to developing osteoarthritis including family history, obesity, previous fractures involving a joint, prior surgery on a joint and overuse.
What treatment options are available to alleviate knee arthritis pain?
- Live with the symptoms.
- Lifestyle modifications including weight loss and avoiding painful activities.
- Physical therapy
- Gait modification tools such a brace, cane, walker, special shoes or shoe inserts.
- Medications including NSAIDs - ibuprofen, Advil, naproxen, Aleve, Celebrex, meloxicam, Mobic or Tylenol.
- Anti-inflammatory diet or supplements such as glucosamine and turmeric.
- Injections such as cortisone (a steroid), Hyaluronic acid (lubricating series), PRP (platelet rich plasma) into the knee joint.
- Total or partial knee replacement to remove damaged cartilage and bone to improve pain and function.
What is a knee replacement?
Your knee is made of three basic parts that work together for the proper function to bend and straighten your leg. Osteoarthritis wears away the cartilage and smooth surface of the bones causing pain and swelling. This eventually leads to joint replacement. Your orthopedic surgeon will consider many factors, such as age, bone density and the shape of your joints to determine the exact kind of knee replacement that is best for you.
Total versus partial knee replacement

If the cartilage in your knee is damaged on both sides of the joint or in all three joint compartments (medial, lateral and under the kneecap), a total knee replacement may be performed.

Knee replacement involves resurfacing the knee joint and using metal and plastic components to replace the damaged tissue. With knee replacement, only a few millimeters of arthritic bone are removed to make space for the new metal endcap. A thick piece of plastic will be inserted between the metal components to act as your new cartilage between the metal. The plastic is contoured in such a way that it mimics the natural motion of your knee. We can improve or correct bow leggedness or knock-kneed malalignment you may have. Dr. Loucks will ensure that your ligaments and your knee replacement work together to give you a very stable, well-balanced knee.
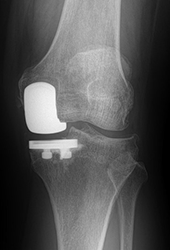
Occasionally, only part of your knee joint will be worn out. Your surgeon may decide that a partial knee replacement is more appropriate for you. The procedure and recovery are very similar to that of a full knee replacement. The downside is that partial knee replacements typically only last 5-10 years before arthritis wears out the rest of your natural knee and it becomes painful once again. This leads to a conversion to a full knee replacement.
Risks of knee replacement
Knee replacement surgery is major surgery, and although advances in technology and medical care have made the procedure very safe and effective, there are risks. These risks should be carefully considered before you decide to have surgery. We encourage you to discuss the potential risks with your surgeon, primary care physician and your family.
Every measure will be taken by our team of experts to minimize your risks and avoid complications. Complications are rare but they do sometimes occur. We will do our best to avoid the most common issues which include:
Blood Clots: Blood clots or deep vein thrombosis (DVT) and Pulmonary Embolism (PE) can develop in a leg vein or in your lungs after joint replacement surgery and are very dangerous. You are at elevated risk for developing a blood clot for a month following surgery so you will likely be on a blood thinner and wear compression socks for a period of time to minimize this risk.
Infection: Infection is very rare in healthy patients. Patients with chronic health conditions such as obesity, diabetes or liver disease are at higher risk of infection after surgery. Superficial wound infections are usually treated with antibiotics. Deeper infections may require additional surgery.
Nerve, blood vessel and ligament injury: Damage to surrounding tissues including nerves, blood vessels and ligaments are possible but extremely rare. Commonly, there is numbness in areas near the incision which usually, but not always, improves in 6-12 months.
Wound healing: Occasionally, surgical incisions heal slowly, particularly if you smoke, are obese, take corticosteroids or have a disease that affects the immune system such as rheumatoid arthritis or diabetes.
Hematoma: Bleeding into a joint can occur immediately after surgery or develop at a later time. This may be accompanied by pain and swelling and can sometimes be confused with infection.
Instability: After surgery, your joint may feel a bit unstable, or you may notice a pop or clicking sensation. This will normally improve as muscles regain their strength, and your body heals the tissues around the new joint.
Wear: Your joint replacement is a mechanical device that will wear over time. The rate of wear may depend on your age, weight, and activity level. Avoiding high-impact activities will extend the life of the implant.
Changes in the Length of your Leg: With knee replacement, leg length is more difficult to control so the operative leg may be a few millimeters longer. Any malalignment (knock-knee or bowleg) may be improved or corrected.
Loosening of the joint: Over the long term, loosening of the artificial joint may occur with wear or if tissue grows between the joint and your bone. This may require revision surgery.
Fracture: Although rare in your skilled surgeon’s hands, fractures may occur at the time of surgery. If this occurs, we may protect your weight bearing for a short period of time or you may require an extended procedure for placement of a plate, screws, or cables to support the bone as it heals.
Malalignment: The alignment and position of your implant is evaluated multiple times throughout your surgery with x-rays and visual inspection. Your surgeon will make every effort to restore natural alignment.
Residual Pain & Swelling: Pain after surgery is normal and expected but should dissipate with time and healing. It may take up to a year for these symptoms to resolve. There may always be some residual swelling and stiffness in a prosthetic joint.
Noise or Squeaking: Painless noises are often normal due to the metal and plastic composition of your implant and will diminish over time. When pain, swelling or deformity are associated with noise, that is a sign your joint needs to be evaluated by your surgeon.
Range of Motion: Within hours of your surgery, you will begin to walk and perform exercises that help improve the strength and flexibility surrounding your new joint. Even after physical therapy and an extended recovery period, some people are not able to regain full motion. Our team will make every effort to minimize the chance of this occurring so that you can perform normal activities with ease.
When will my new joint wear out?
Starting with your first step, the plastic bearing between the metal parts begins to wear. We know it is quite durable and should last decades, but it still wears over time. If the plastic wears out enough, the ligaments become slack and a feeling of instability results.
If you experience a lot of swelling, pain or giving way, you may require a revision surgery. We will perform some tests to determine what needs to be replaced. Many times, it is only the plastic part that needs replaced and that procedure is a much easier recovery than the index surgery. Out of 55,000 knee replacement patients, only 3.9% required a revision surgery within 10 years. By 20 years, 10.3% required a revision, according to a 2017 article in Lancet. It is hard to predict what type of problem you might have in the future some come see us if you have any issues.
I have a Baker’s Cyst. Will it go away after knee surgery?
A Baker’s Cyst is a pocket of fluid behind the knee. It is extremely common and is not harmful or dangerous. This is rarely a source of pain although some patients have some discomfort if it fills with a lot of fluid. Nearly everyone over age 50 has one, and they vary in size. They are the result of knee conditions such as arthritis or cartilage tears. When the inside of the knee has some damage, the lining of the knee makes extra fluid. That fluid can squeeze out between the calf muscles and hamstrings, resulting in a reservoir of extra fluid. The area can bulge causing a tight feeling behind the knee. They can get bigger and smaller depending on how inflamed your knee is. We used to drain these cysts but no longer do so because they come right back the next day since the underlying problem (arthritis or cartilage damage) didn’t get addressed. By having a knee replacement, we remove the offending arthritis, but the cysts generally do not go away completely. They do get much smaller 6 months after surgery.
Implant Information – Knee Replacement
Every patient is different, however, if this is the first joint you have had replaced, more than likely, we will use an implant made by Medacta. Dr. Loucks trusts the products made by Medacta and has been using their hip and knee implants since 2008. If you have had your joint replaced previously and need it revised, your surgeon may choose to use components made by a different manufacturer.
Medacta International is the innovative maker of our Total Hip and Total Knee Implants. Their motto is “Quality in Motion” and their goal is to allow patients to regain a healthier and more active lifestyle. Medacta is one of the fastest growing orthopedic implant companies over the past 25 years. Medacta is based in Switzerland and is represented in 60 countries worldwide. For more information, visit www.medacta.com.
The majority of our Total Knee Replacement patients will have the Medacta GMK Sphere Implant.

The GMK Sphere is a cutting-edge, “ball-in-socket” medial-stabilized knee implant that is tailored to each individual patient. Based on knee anatomy and overall limb alignment, the CT images of your knee allow your surgeon to have a 3D model of your bone and a patient-specific cutting guide that he uses during your surgery. The “ball-in-socket” design has many benefits:
- Patients report that “It feels more normal” than traditional knee replacement designs.
- Patients report that it feels more stable with mid-flexion activities such as ascending or descending stairs, squatting, skiing, and golf.
- It allows more normal motion with rotation during flexion and loading of the joint.
- Most traditional total knee replacements that sacrifice the ACL and PCL require a plastic post to control front to back stability. The Sphere does this with the Medial “ball-in-socket” design so there is frequently fewer clunks and pops.
Following your surgeon’s preferences and utilizing the CT scan, the engineers can create a virtual 3D bone model of your knee joint. Using the virtual model, the cutting guide is positioned on your knee. Your surgeon can modify the positioning as he wishes. Once the pre-operative plan is approved by your surgeon, the manufacturing process begins, and your implant is shipped to your surgeon in time for your surgery.
- The metal implant is made of surgical stainless steel including a cobalt-chrome alloy.
- The plastic component is a machined ultra-high molecular weight polyethylene.
There are many advantages to using the MyKnee system:
- There is more accurate sizing and implant positioning on your bone.
- Fewer surgical steps, which leads to shorter surgical time and less time under anesthesia.
- There is less blood loss and less risk of blood clot/embolism due to no intramedullary canal violation.
- We can apply Kinematic Alignment Principles to insert your new knee.
What is Kinematic Alignment (KA) in Knee Replacement?
In general, total knees are implanted using either Mechanical Axis (MA) alignment OR Kinematic Alignment (KA) Principles. Historically, most total knee replacements were implanted using the mechanical axis method. This method basically cuts every patient’s knee at the same angle. In other words, the bone cuts around the knee are intended to effectively make every patient’s knee/leg perfectly straight.
The trouble with this approach, is that we know from decades of research and doing knee replacements, along with the CT scan data of tens of thousands of knee patients, that most patients legs are NOT perfectly straight. Many patients are varus (bow-legged) for most of their life, while some are valgus (knock-knee). The soft-tissues, ligaments, and patella (kneecap) are used to functioning at these pre-existing positions and angles. If we ignore these angles (Mechanical Axis Alignment) and cut every patient perfectly straight, a certain percentage of these patients continue to have pain, swelling and trouble with their knee replacements despite our best efforts.
For these reasons, we have transitioned over the years towards Kinematically Aligned (KA) Total Knee Replacement. Dr. Stephen Howell, our friend and colleague, has been instrumental in teaching knee surgeons around the world the benefits of Kinematically Aligned Total Knee Replacement. Since 2015, we have been following these KA principles and have seen a tremendous benefit in our patients.
In Kinematic Alignment Total Knee Replacement, we insert the knee in the EXACT position that matches the position of the native knee BEFORE the patient developed arthritis. Effectively, we remove the exact same thickness of bone that matches the thickness of the new metal knee placing the new metal knee in the same position of the original knee. We use our pre-operative CT scan to assist with this planning, however, we have specialized instruments and measuring devices that allow us to do it in the event we cannot get a CT done before surgery. We literally measure each small cut of bone to the millimeter to ensure an accurate reconstruction!
What if I have an allergy to metal?
On occasion, we have patients that report an allergy to metal or specific metals that are used in our implants. Most of these patients have no issues with these implants. Just because your skin has a positive “patch test” does not mean you will adversely react to the alloy in these implants. We will sometimes utilize Medacta’s SensiTiN knee that has a ceramic-like coating of titanium nitride that is designed to reduce the release of metal ions. If you have metal allergy concerns, discuss this with your surgeon. We may discuss the latest scientific evidence and can provide literature from the American Association of Hip and Knee Surgeons (AAHKS) if requested.